Unlocking the Potential of TMS for Stroke Recovery: A Breakthrough in Neurotherapy
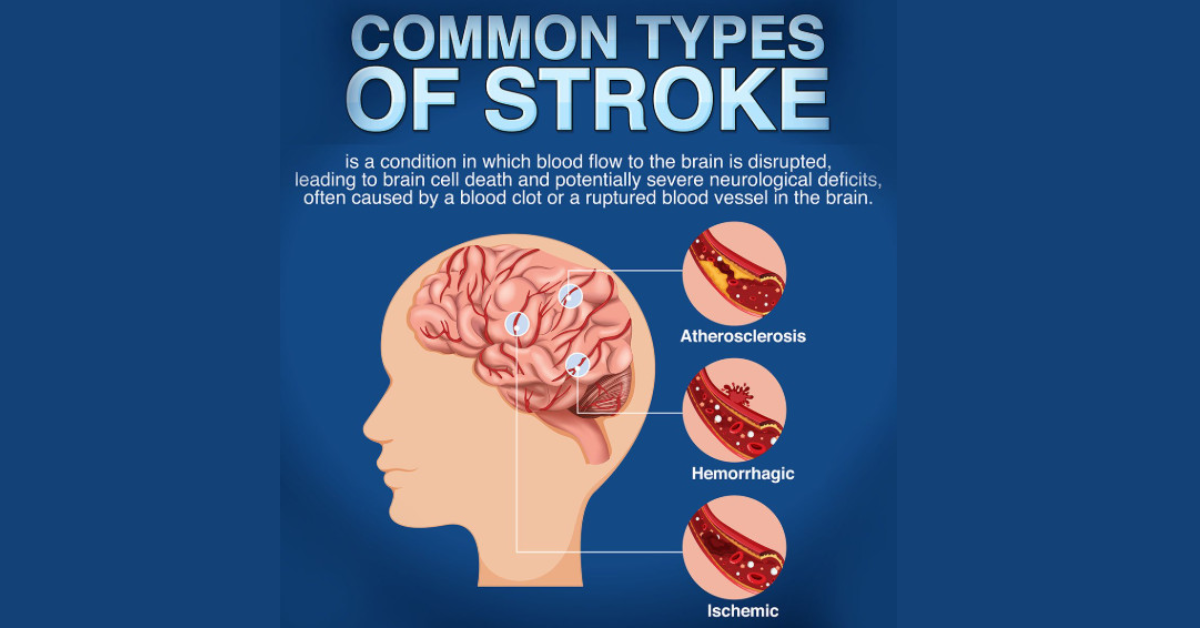
TMS For Stroke: Stroke remains one of the leading causes of disability worldwide, affecting millions of individuals every year. While traditional recovery methods such as physical therapy, medication, and surgery have been the standard, recent advancements in non-invasive therapies are offering new hope for stroke survivors. Among these, Transcranial Magnetic Stimulation (TMS) has emerged as a revolutionary treatment. Specifically, TMS therapy using permanent magnets (TMS-PM) offers a promising approach to stroke rehabilitation. This article explores the science behind TMS for stroke, its benefits, and how it’s transforming recovery.
What is Transcranial Magnetic Stimulation (TMS)?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. By targeting specific brain regions, TMS helps enhance brain activity, facilitating neurological recovery. It has been used primarily for treating mental health conditions like depression and anxiety. However, its applications are expanding, particularly in the field of stroke rehabilitation.
How TMS Works for Stroke Recovery
The basic principle behind TMS for stroke revolves around the stimulation of targeted brain regions that are affected by a stroke. A stroke often leads to damage in areas of the brain responsible for movement, speech, and cognitive functions. When these regions are impaired, individuals may experience paralysis, speech disorders, or cognitive decline. TMS works by stimulating these damaged areas, helping to rebuild neural connections and improve brain function.
In the case of stroke patients, TMS can be applied to areas such as:
-
Motor Cortex: For improving motor skills and movement in limbs affected by paralysis.
-
Broca’s Area: For aiding speech recovery in stroke survivors with aphasia or mutism.
-
Prefrontal Cortex: For addressing cognitive issues, such as attention and memory problems.
The stimulation from TMS encourages neuroplasticity—the brain’s ability to form new connections—which is crucial in stroke recovery.
The Benefits of TMS for Stroke
-
Enhanced Motor Function: One of the primary benefits of TMS in stroke recovery is the improvement in motor function. Stroke patients often experience limited mobility due to the damage to their motor cortex. Regular TMS therapy can stimulate the motor cortex, encouraging the brain to create new pathways and restore movement in the affected limbs.
-
Speech Recovery: Stroke survivors with speech disorders such as aphasia can benefit greatly from TMS. Targeting areas like Broca’s area, which is responsible for speech production, helps facilitate recovery by promoting neuroplastic changes that aid in regaining speech.
-
Cognitive Improvements: Many stroke survivors also struggle with cognitive impairments, such as memory loss and reduced attention span. TMS therapy, by stimulating the prefrontal cortex, can improve cognitive function, making it easier for patients to process information and regain their mental clarity.
-
Non-Invasive: Unlike surgical interventions, TMS therapy is non-invasive, meaning there is no need for incisions or anesthesia. This makes it a safer and more comfortable option for many stroke survivors.
-
Minimal Side Effects: TMS therapy is generally well-tolerated by patients. The most common side effects are mild headaches or scalp discomfort, which usually subside shortly after treatment. This makes it a preferable option compared to more invasive procedures that might involve longer recovery periods or higher risks.
TMS-PM: A Game-Changer in Stroke Rehabilitation
TMS-PM, or Transcranial Magnetic Stimulation by Permanent Magnet, is an advanced form of TMS therapy. This innovation uses a permanent magnet to stimulate the brain, providing an accessible and cost-effective treatment option. The device is portable, simple to use, and can be administered by the patient at home, under the guidance of a healthcare professional.
One of the key advantages of TMS-PM is its affordability. Unlike traditional TMS devices that can cost thousands of dollars, the TMS-PM device is priced at a fraction of the cost, making it accessible to a wider range of patients. For stroke survivors, this means more affordable and consistent access to neurotherapy.
TMS-PM for Stroke and Paralysis
Stroke-induced paralysis can be one of the most debilitating effects of the condition. However, TMS-PM for stroke shows promising results in improving motor function, particularly in the arms and legs. By targeting the bilateral motor cortex, TMS-PM stimulates the areas responsible for muscle movement and coordination, which helps stroke survivors regain function over time.
Research and clinical trials have shown that TMS-PM can reduce the severity of paralysis, improve limb mobility, and enhance overall quality of life. This therapy has been successfully used to treat both upper and lower limb paralysis, with patients showing significant improvements in their ability to move.
The Role of TMS in Post-Stroke Rehabilitation Programs
Post-stroke rehabilitation often involves a combination of therapies aimed at restoring lost functions. These include physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation. TMS therapy can complement these traditional rehabilitation approaches by accelerating the healing process.
-
Physical Therapy: When combined with TMS therapy, physical therapy outcomes are enhanced as the brain is encouraged to rewire and strengthen motor pathways more quickly.
-
Speech Therapy: Stroke survivors with aphasia can benefit from TMS therapy by stimulating the brain regions responsible for speech, making speech therapy more effective.
-
Cognitive Therapy: TMS can aid cognitive recovery by targeting the brain regions responsible for memory, focus, and problem-solving, accelerating cognitive rehabilitation efforts.
The Science Behind TMS for Stroke
The mechanism of action of TMS involves the application of a magnetic field that induces small electrical currents in the targeted brain regions. These currents help stimulate neurons, promoting brain plasticity and encouraging recovery. TMS has been shown to improve functional outcomes in both chronic and acute stroke patients.
Research indicates that TMS can improve brain activity in the affected regions, facilitating communication between neurons and supporting the rehabilitation process. Over time, with consistent therapy, these effects lead to tangible improvements in mobility, speech, and cognition.
FAQ: Frequently Asked Questions About TMS for Stroke
1. How long does it take to see results from TMS therapy?
The results of TMS therapy can vary from patient to patient. Typically, patients start seeing improvements within 1 to 3 months of regular therapy sessions. However, continued use over a period of 6 to 12 months may lead to more significant results.
2. Is TMS therapy safe for stroke patients?
Yes, TMS therapy is generally considered safe for stroke patients. It is a non-invasive procedure with minimal side effects. However, it is important to consult a healthcare provider before starting TMS therapy to ensure it is appropriate for your condition.
3. How often do I need to undergo TMS therapy?
The frequency of TMS therapy depends on the individual’s specific needs and the severity of their stroke. In most cases, patients undergo therapy 3 to 5 times a week, with sessions lasting about 20-30 minutes each. A typical treatment duration is 3 to 6 months.
4. Can TMS help with speech disorders caused by stroke?
Yes, TMS has been shown to help with speech disorders, such as aphasia, by stimulating the areas of the brain responsible for speech production. Regular TMS therapy can improve language skills and help stroke survivors regain the ability to communicate.
5. Is TMS therapy covered by insurance?
Coverage for TMS therapy varies depending on the insurance provider and the region. It’s best to check with your insurance company to determine if TMS therapy is covered under your plan.
6. Can I use TMS-PM at home?
Yes, TMS-PM is designed to be used at home under the supervision of a healthcare provider. The device is portable, easy to use, and affordable, making it an accessible option for stroke patients seeking home-based therapy.
Conclusion: A Bright Future for Stroke Survivors
The use of TMS for stroke recovery represents a significant advancement in neurotherapy. With its ability to stimulate brain regions, promote neuroplasticity, and improve motor, speech, and cognitive functions, TMS offers stroke survivors a powerful tool for recovery. The introduction of TMS-PM makes this therapy even more accessible, giving patients a cost-effective, non-invasive treatment option that can accelerate their recovery journey. As research continues to evolve, the potential for TMS therapy to revolutionize stroke rehabilitation is immense, offering hope to millions of individuals worldwide.